Emergency medicine: ACLS compendium
This article has originally been published in Norwegian. This is a machine translated version of it, be aware that the terminology might not be correct:
ADVANCED CARDIOPULMONARY RESUSCITATION (AHLR) COMPENDIUM
Revised March 2017
Copyright
Chief physician, Prof JK Heltne, Akuttmed.avd/KSK, Helse-Bergen and the University of Bergen, jkhe@helse-bergen.no
Senior doctor Eirik Alnes Buanes, intensive care physician. Section/KSK Helse-Bergen HF, eabu@helse-bergen.no
Reprinted with permission from Jon-Kenneth Heltne for use by people with some prior knowledge.
Contents:
- Introduction
- AHLR - Status quo
- What causes cardiac arrest?
- Detect cardiac arrest. Notification.
- The priority list
- The treatment algorithm
- After resuscitation
- Appendices and references
1. I ntroduction
This compendium in advanced cardiopulmonary resuscitation (AHLR) has been prepared by the Department of Emergency Medicine, KSK, Helse Bergen. The content is based on our understanding of Norwegian and European guidelines from 2015 and on the Department of Emergency Medicine's internal AHLR training. If you are going to participate in an AHLR course, it is expected that you have read this compendium first. For those who wish to delve further into AHLR, one of NRR's AHLR courses is recommended.
It is desirable that everyone knows basic cardiopulmonary resuscitation (CPR), which is resuscitation without aids (other than a face cloth or pocket mask), and can also use a defibrillator (= defibrillator). We build on BHLR in this compendium.
Advanced cardiopulmonary resuscitation (AHLR) also involves advanced handling of the airways and drugs.
2. AHLR - Status quo
• It is approx. 4,000 cardiac arrests annually in Norway, 2/3 of which occur outside hospitals.
• Survival after cardiac arrest is 2-20% (large gap in this figure because it depends on which types of cardiac arrest are included in the data collection and follow-up afterwards).
• Up to 3 times as many survive with good quality CPR, but fewer than 50% perform good and acceptable CPR!
Myth about sudden cardiac arrest: "- Sudden cardiac arrest only affects older people.
They get a short-lived and needy life!”
BUT:
- The average age is approx. 63 years.
- 3/4 of those who survive achieve the same function as before the cardiac arrest.
- Those discharged from hospital live almost as long as comparable patients.
Current European guidelines were revised in 2015. The changes this time focused on simplifying the guidelines and further focusing on factors that matter for survival.
Our most important challenge is to ensure that the right measures are taken in the right order.
Three factors that we know increase survival:
- quick start-up and good quality of CPR
- early defibrillation
- good treatment after the heart has started (post-resuscitation treatment)
Within trauma care, ABC has established itself as a good rule to remember. We want you to be left with a priority list for AHLR:
- COMPRESSIONS
- DEFIBRILLATION
- AIRWAY MANAGEMENT
- MEDICINES
The points are discussed in more detail under chapter 5 Treatment.
3. What causes cardiac arrest?
About. 80% of all cardiac arrests are due to disease in the heart itself (cardiac cause). After a heart attack, there is a high risk of conduction disturbances such as ventricular tachycardia (VT) or ventricular fibrillation (VF). VT and VF will in the vast majority of cases require a shock with a defibrillator to be able to switch to a pulsatile rhythm (ROSC = Return of spontaneous circulation). The heart can also have such fatal electrical conduction disturbances without a heart attack.
Ventricular tachycardia (VT) is a regular rhythm disturbance, but if it is fast enough (usually over 180/min), it will lead to unconsciousness and loss of pulse because the heart is unable to work efficiently.
Ventricular fibrillation (VF) can be described as electrical chaos. It is a very energy-intensive process. In the first few minutes, many electrical heart cells are active, that is to say large changes in the electrocardiogram (ECG) and a "rough fibrillation". Eventually, when the heart cells do not get enough nutrition, the beats become smaller - "fine fibrillation".
Ventricular fibrillation causes uncoordinated contractions in the heart muscle (the heart "flickers"), thus not providing circulation and causing immediate unconsciousness.
Asystole (AS) is when the heart is completely still and there are no electrical impulses in the heart. EKG is completely flat. When this is the initial rhythm, you must remember to check that the defibrillator is working.
Pulseless electrical activity (PEA). Electrical impulses can be read in the EKG, but there is no palpable pulse (no or poor pump function). The curve that is registered may resemble the curve for a pulsatile rhythm. It is therefore only you who can decide whether it is a PEA or a pulsatile rhythm. You do this by feeling for your pulse.
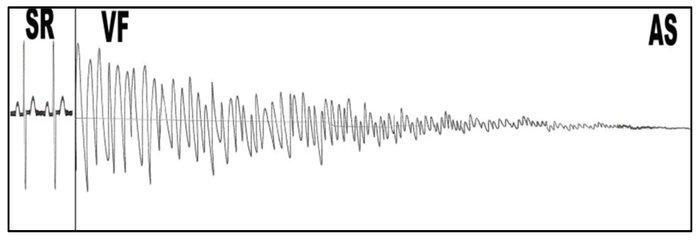
Figure 1. SR-VF-AS. The image shows a possible course of untreated cardiac arrest. From an initial organized rhythm, a coarse VF occurs. Eventually, the fibrillation will become progressively finer and turn into an asystole.
In the first minutes after a cardiac arrest, the heart will fill up with blood. This happens because there is still some pressure in the veins and the blood is pushed back to a heart without the ability to pump away. This causes the heart to grow and it is less susceptible to defibrillation. Cardiac compressions are therefore both "buying time" until a defibrillator arrives and a preparation of the heart (emptying of blood) so that it is more susceptible to shock.
About 20% of all cardiac arrests are not due to heart disease (non-cardiac cause).
The rule to remember here is the four H's and the four T's:
- Hypoxia. Too little oxygen is offered to the blood from the lungs. When the airways are blocked (e.g. suffocation, foreign body, drowning), CO poisoning or asthma/COPD, the lack of oxygen eventually leads to cardiac arrest.
- Hypovolemia. Not enough blood volume to pump and thus lack of oxygen transport. Large internal or external bleeding can lead to circulatory failure and circulatory arrest.
- Hypo/hyperkalemia. Large changes in potassium in the blood disrupt the electrical conduction in the heart. Prolonged vomiting/diarrhea or the use of diuretic drugs can result in low potassium. Untreated kidney failure is the most common cause of high potassium. Both disturbances can cause rhythm disturbances and cardiac arrest.
- Hypothermia. Cooling makes the heart generally more susceptible to rhythm disturbances. Patients may initially have a slow pulse and breathing. It can be easy to overlook signs of life. Cooling before the cardiac arrest can give a better prognosis. All patients with cardiac arrest due to hypothermia must be considered transported to hospital for rewarming on a heart-lung machine.
- Tamponade. Leakage of blood between the heart and the membrane that surrounds the heart. The blood compresses the heart from the outside. This can be due to leakage from the heart (after a heart attack), or via sharp or blunt force to the heart (shots/stabs/falls/car accidents). This causes an acute pump failure.
- Pressure pneumothorax. Air between the lungs and pleura (pneumo = air, thorax = chest). This can happen when the lungs are punctured or by gunshot/stab wounds that go through the chest wall. The lung then completely or partially collapses. If a valve mechanism occurs that allows air to enter but not exit, an increasingly high pressure builds up in the chest (pressure pneumothorax) and blood does not return to the heart.
- Thromboembolism. A large part of a blood clot in a vein can dislodge and travel via the heart and block one of the pulmonary arteries. The patient will quickly have circulatory arrest as a result of the change in the pressure conditions in the heart.
- Toxins. Poisonings can affect circulation, the heart or respiration (e.g. hypoxia/respiratory arrest after an overdose with heroin and tricyclic antidepressants which can cause a drop in blood pressure, arrhythmias or respiratory arrest).
4. Detect cardiac arrest. Notification.
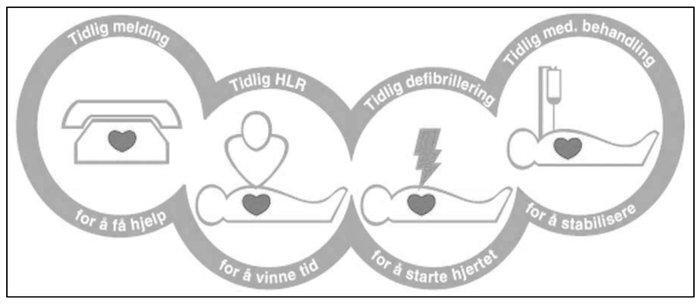
Figure 2. The chain that saves lives
The chain that saves lives:
The chain shows several measures that must all be carried out as soon as possible after a cardiac arrest. The chance of survival decreases by 7 - 10% for every minute that passes without treatment.
- Early notice. Early understood danger signal and alarm. In the first hours after a heart attack, the risk of cardiac arrest is greatest. By recognizing signs of this, notification to 1-1-3 will shorten the response time for emergency medical help.
- Early basic cardiopulmonary resuscitation. Early initiation of good CPR in cardiac arrest increases the chance of survival 2-3 times. Avoid all unnecessary pauses in the compressions.
- Early defibrillation. Delayed defibrillation in cardiac arrest significantly reduces the chance of survival.
- Early advanced treatment and good post-resuscitation care. Advanced airway measures and the use of drugs during resuscitation have not been shown to increase survival. Therefore, focus on effective CPR and early defibrillation. Good monitoring and preparedness, as well as diagnostics and advanced treatment in hospital increase survival.
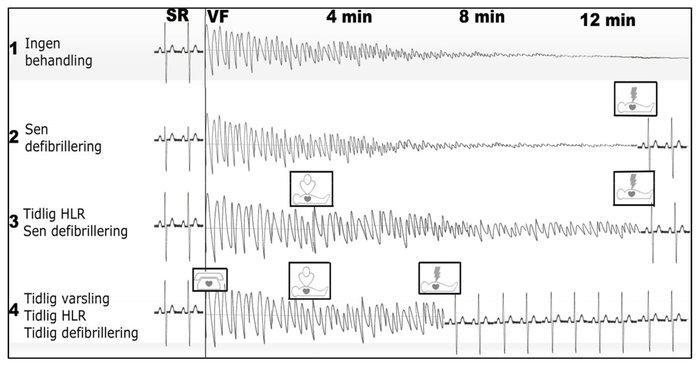
Figure 3. The effect of a functioning Chain of survival
Figure 3 illustrates the importance of the "chain that saves lives" and shows imaginary examples of registrations after cardiac arrest. The top line (1) shows what happens if the person does not receive treatment at all. From a normal sinus rhythm, the patient first has a coarse VF, we progressively finer VF to an AS. The second line (2) shows what happens if we try to defibrillate a fine VF; very low probability of success. The third line (3) shows what happens when you start CPR early, but have a delayed defibrillation. Then you keep a rough VF for longer, but still have a fairly low probability of success. The last curve (4) shows early warning, early initiation of CPR and early defibrillation. Here you have the greatest opportunity to get the heart going again.
5. The priority list
1. COMPRESSIONS
Optimal compressions can provide up to 25-30% of normal circulation. This is a minimum of the circulation that is needed to prevent permanent damage to the brain and heart. It is therefore crucial for the patient's prognosis that we focus on the compressions being done correctly. At least 7-8 consecutive compressions are required before you have "built up enough pressure" to get circulation. Every time you make a pause in the compressions, the circulation quickly drops to 0. Each such pause in the compressions, as long as the heart is not beating itself, is called "hands-off time". This time must be reduced to a minimum to maintain the marginal blood flow we can achieve with compressions. All unnecessary hands-off time reduces the patient's chance of survival!
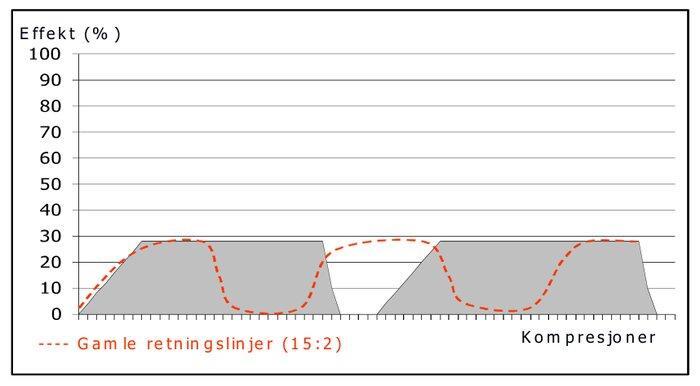
Figure 4. The gray box shows that after 6-8 good compressions you achieve up to 25-30% of the effect compared to if the heart was beating on its own. As soon as you stop compressing, blood flow drops immediately. The dashed line shows that old guidelines gave significantly longer hands-off time.
There are five things you should think about to give good compressions:
- Placement. Sit close to the patient. Place the back of one hand in the middle of the patient's sternum, in the middle between the nipples. Put the other hand on top and "interlace your fingers". Keep your arms straight and try to get well over the patient.
- Depth. The compressions should be deep enough, the ideal is 1/3 of the chest height from the floor when the patient is lying on his back. This corresponds to 5-6 cm on an adult man. If you break the rib, you are compressing too hard. If you break a lot of ribs, the effect of the chest compressions decreases.
- Frequency. You must compress at least 100 times per minute. If you compress too quickly, it will be difficult to provide good compression. A frequency between 100 and 120 per minute is recommended. This means that you should use 15-18 seconds for 30 compressions. It will be easier for your colleague if you count out loud. Feel free to increase the volume of your voice when you approach 30, so that your partner gets ready for inhalations. You can give the first compression when the chest rises on the second inhalation, so that the hands-off time is as short as possible. When you say "30" and give the last compression, the partner gives the first breath. It takes training to achieve such good transitions when doing CPR. Do not wait if the partner is not ready to inhale - then you continue the compressions. After the partner has secured the airway with a tube, you must switch to continuous compressions (without stopping for breaths). Then it is most appropriate to count to ten, and then start at one again. It is to remind the partner that he/she gives a breath every ten compressions.
- Avoid "leaning". Remember that you must let go completely between each compression. If you hold and do not release the pressure on the chest all the way up, we call it "leaning". It reduces the effect of the compressions. The heart receives blood during diastole (when the heart relaxes) and the brain receives blood during systole (when the heart beats), this is also the case during compressions. The coronary arteries in the heart fill with blood when you let go between each compression.
- Smooth compressions. Try to spend the same amount of time on compression as on decompression. You will work like a piston in an engine. Avoid breaks at the top or bottom. Avoid "hitting" the compressions into the patient, work evenly!
If you are not the one providing the compressions, you must use these five points to give feedback to the person doing the compressions. That way, you can help ensure that the compressions are good enough. It is advisable to change the compressor every 3 minute cycle if practical. Doing good compressions on an adult is very difficult and it does not take many cycles before one person alone is unable to maintain the correct depth.
Once cardiac arrest has been established, CPR should be started as soon as possible. If there are others who alert, start BHLR 30:2. If a defibrillator is present, you can give continuous compressions until it is ready for analysis.
2. DEFIBRILLATION
The defibrillation shuts down all electrical activity, so that the heart has an opportunity to restore synchronized electrical impulses.
The chance of being discharged from hospital alive drops by 7-10% for every minute that defibrillation is delayed after cardiac arrest (if CPR is not performed. It is therefore essential that you switch on and connect the defibrillator immediately after cardiac arrest has been detected. Start continuous compressions or CPR 30:2 until the defibrillator is ready, it improves the prognosis and increases the chance of own heart rhythm after shock!
The electrodes are placed so that as much current as possible passes through the heart. If the electrodes are placed correctly, only 10% of the current still passes through the heart. Look at the adhesive electrodes where they should be placed, it is not a big mistake to switch if the placement is mutual. One is placed up in the "angle" that forms between the sternum and the right collarbone. The other is placed a hand's width below the left armpit, and should be as much over the back as on the front of the chest (midaxillary line).
Remember rescuer and patient safety during defibrillation!
You must know the equipment you use in detail. It is too late to read the instructions for use when you see the ventricular fibrillation on the screen.. Learn to use the defibrillator, be sure which buttons to press - even if something does not go as planned.
Check the defibrillator regularly.
Defibrillators
Newer defibrillators are biphasic. That is, they send the current through the heart first in one direction, then in the opposite direction. This has proven to be more effective than the old defibrillators, which send the current only one way (monophasic). This means that the amount of energy used in biphasic defibrillators can be reduced, and the damage to the heart is reduced. The exact strength that is selected depends on the brand of the defibrillator. Monophasic defibrillators are less effective.
Manual defibrillators give the rescuer the opportunity to choose the current strength and whether to give a shock. Most manual defibrillators can also be used in semi-automatic mode, as the defibrillator itself decides whether to give a shock. The defibrillators hanging around shopping centres, airports and sports arenas are simple, semi-automatic or fully automatic defibrillators. The fully automatic ones themselves decide whether to give a shock, charge up and deliver the shock without the rescuers having to press anything other than the on button.
Only VF and VT should be shocked and are called shockable rhythms. A successful shock changes the rhythm, usually to AS or PEA/sinus rhythm. This is also called converting. AS and PEA should not be given a shock. Fine VF is treated as AS, as there is little probability of converting a fine VF.
Therefore, many shopping centres, sports arenas and public installations are equipped with an automatic or semi-automatic defibrillator. There is no longer a requirement for delegation from a doctor to use such a defibrillator, but one should have taken a course in defibrillation CPR first.
In severely cooled patients (tp < 30 degrees) and at the same time a shockable rhythm, one should not defibrillate more than three times, because the patient may be too cold for the heart to start again and one should avoid damaging the heart. These patients must be taken to hospital under ongoing CPR and warmed up in a controlled manner before possibly giving up the resuscitation attempt. Do not start the active heating during transport.
After a successful shock, you may not get a pulse-generating rhythm. Of the hearts that get a pulsating rhythm after a shock, only approx. 10% that gives a pulse directly after the shock. The remaining 90% start within the first minute. We therefore do not wait to see if the heart starts again after a shock, we start CPR immediately. After one minute after a shock, we take a short pulse check and look at the EKG one screen width to pick up those who have acquired a pulse-giving rhythm. The only reason to stop CPR then is if you feel a pulse.
3. AIRWAY MANAGEMENT
Airway management is a difficult task. Use a technique you master. To begin with, it may be a good idea to use a pocket mask connected to oxygen and give inhalations with this. If you encounter problems maintaining a clear airway when inhaling with a pocket mask, you should insert a throat tube.
Blow in calmly, each inhalation should take approx. one second. You should see your chest rising with each inhalation and then falling again afterwards. Do not give another breath until the air has been released from the lungs. When you see your chest rise, you have blown enough. Then you know that the lungs are so full of air that they expand the chest. If you blow further or very forcefully, there is a great risk that part of the air will go down into the stomach. This will gradually fill with air. This increases the risk of the air, and accompanying stomach contents, coming up the throat and being carried down into the lungs. This is called aspiration.
Ventilation with a self-expanding bag and mask is a demanding technique. It is difficult enough in calm conditions, and it becomes almost impossible to do this well in a cardiac arrest situation. In that case, this locks the person to focus only on whether the chest rises and that the mask does not leak. You have much better control with a pocket mask.
If you have used a laryngeal tube, laryngeal mask or equivalent supraglottic airway, your hands are freed. You can then ventilate the patient using a self-expanding bag connected to high-flow oxygen. The patient then receives 100% oxygen. A big advantage of this is that you can do continuous compressions and "trick in" ventilations between the compressions. This saves you hands-off time for doing inhalations. A common way to ventilate is to give one breath for every 10 compressions.
When you use respiratory aids, you reduce the risk of stomach contents finding their way to the lungs. The tubes also give you the opportunity to suck out air and liquid from the stomach using a catheter (tube) and a suction. An empty stomach gives better room for the heart so that the heart is better able to receive venous blood from the body.
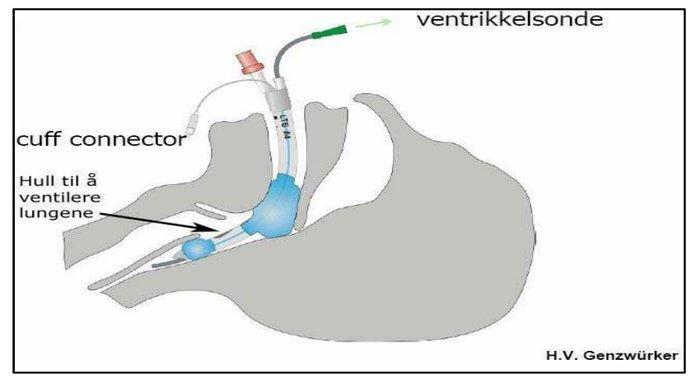
Figure 3. If you are trained to use a supraglottic device, e.g. laryngeal tube/laryngeal mask/I-gel, it is a good way to establish the airway. Helse Bergen has this as the first choice for securing the airway in the ambulance service
To evaluate whether the tube is in place, there are four points that can help you:
- "The good feeling". This is the feeling that you are in place when you put the tube down. For the laryngeal tube, this means that it "sets down" and that it rises a little when you fill the cuff with air. For the endotracheal tube, this applies that you see it pass the vocal cords.
- Breast lift. That the chest rises during inhalation and then lowers afterwards is a sign that the tube is positioned correctly. If you have used an endotracheal tube, you must also see if the chest rises equally on both sides.
- Result on CO 2 detector. Color cover on Easy-cap or capnograph that gives results. These register Co 2 in the exhaled air of the patient. Easy-cap or capnograph should ALWAYS be used if an airway is closed.
- Auscultation. Listening with a stethoscope first over the stomach and then over both lung surfaces. It pays to listen a little louder than expected, since the stomach may be inflated if CPR was performed before you arrived at the patient. Therefore, listen just below the end of the tip of the sternum and in the armpits/upper part of the chest on both sides. You cannot listen during compressions, and you must not interrupt compressions to listen (compressions are higher on the priority list than airways...). The only opportunities you have to listen are therefore just before and just after the analysis (not during the analysis, because then the chest must lie completely still).
Constantly evaluate whether you are getting air in the patient! If you are unsure or not completely satisfied, you should choose a simpler technique, not a more difficult one. If in doubt - remove the tube and go for a simpler technique. Remember to fix the tube with duct tape, tape or tube fixation made for the tubes.
4. MEDICATIONS
Medicines are only allowed to be considered when you have control over the three highest priority measures; compressions, defibrillation and airways. It will therefore be practically impossible to insert an IV before the airways are secured, if there are only two rescuers present.
No drugs used in cardiac arrest have shown increased survival. This implies that there should be a low focus on drugs. However, we know from animal studies and from using the drugs on living people that they can have an effect. Perhaps they have not shown increased survival because the use of drugs takes the focus away from what we know saves the patient: good compressions and optimally timed defibrillation.
An intravenous access (venflon) must be placed as centrally as possible, no further out on the arm than the elbow. The jugular veins can be used if they are clearly visible. Hang up a Ringer's Acetate (RA, intravenous fluid) early, so you don't have to draw up fluid every time to flush after when you put a drug. Intraosseous access is an alternative if you are unable to obtain intravenous access.
Adrenaline is the drug that is prioritized first. 1 mg is administered approximately 1 minute into each three-minute cycle after intravenous access has been established. If you have given a shock, you must wait until after you have checked the pulse (1 minute out of the loop) before giving the medication. It can be very unfortunate to give 1 mg Adrenaline to a heart that has just been shocked to start again.
Cordarone 300mg can be given undiluted after 2 shocks if the rhythm is still shockable (VF or VT). Stop the RA infusion while instilling the drug. The medication can be repeated in half the dose (150mg) if it has no effect. Adrenaline is prioritized before Cordarone. It is also important to consider alternative electrode placement and whether the patient is severely cooled, if the shocks are unsuccessful.
6. The processing algorithm
It is natural that the rescuer with the most experience is present to examine the patient and take care of the airways. These are the tasks that require the most experience and knowledge. At Helse Bergen, we call this person the "head man". In an extreme situation, where there are only two rescuers present, it is natural that the other rescuer takes care of both compressions and defibrillation - "defi-man". This person then gets the two most important tasks and must not have other tasks. This means that the head man must take care of everything else.
When you arrive:
1. Consider security. The personal safety of rescuers and relatives is the first priority. Avoid the tragic situation being extended to harm or kill others.
- Assess whether the surroundings are safe for the rescuers and enable safe and effective treatment. Move the patient if necessary.
- The risk of infection from the patient when using a pocket mask with a one-way valve is almost negligible. Use a face cloth for mouth-to-mouth.
- Use disposable gloves.
- Be aware of the danger of defibrillation. No one should touch the patient when a shock is administered. Dry the skin and shave away hair. Use adhesive electrodes that reduce the risk of arcing between the electrodes. Put away oxygen equipment during defibrillation (NB! Increased risk of ignition of gas in a closed space).
- Use yellow boxes for used tips.
2. Take the lead. Be clear and definite. Use "closed loop orders", that is, the person who is told to do something repeats the message out loud. That way, both know that the message has been understood.
3. Determine cardiac arrest.
- Talk to the patient, possibly shake him/her gently. Call for help if there is no response.
- Place the patient on his back.
- Take a strong jaw grip (or bend the head back if you do not suspect a neck/back injury) to check consciousness and provide a clear airway.
- Listen and feel for breathing with the ear, while looking at the chest for breathing movement. Remember to still maintain a clear airway.
- If the patient is unconscious and not breathing normally, you have established cardiac arrest.
- Warn. Call 1-1-3 yourself or have someone else do this. In addition, notify any other resources that are closer.
- Start with five breaths in patients in whom hypoxic cardiac arrest is suspected, continue with 30:2.
- Start CPR!
Be aware that patients who go into cardiac arrest may have "agonal gasps" a little while after the heart has stopped. This is not regular, efficient respiration and they are not breathing normally.
1. Determine cardiac arrest, get help and start CPR 30:2
2. Immediately when available: Switch on the defibrillator and attach the electrodes without interrupting CPR.
3. Assess good CPR for three minutes. before the first shock.
4. Analyze the heart rhythm
- Always feel for pulse at the same time as analysis, start CPR immediately (without analysis
- If shockable rhythm (VF/VT): Give shock no. 1 or feel the pulse) and continue for three min. analyze the rhythm if still give shock no. 2 start CPR immediately and continue for three minutes. shockable rhythm analyze the rhythm etc.
- If AS / fine VF: Start CPR immediately (without pulse sensing) and continue for three minutes. analyze the rhythm etc.
- If "organized" non-shockable rhythm: if no pulse (PEA) start CPR immediately, analyze the rhythm etc. and continue for three min.
5. Intubate only if you are specialist personnel
- After intubation: Continuous compression + 10 breaths/min
- Connect the capnograph or Easy-Cap to the tube
6. Insert venflon and give drugs when it is practically possible.
7. Consider correctable causes (the four H's and the four T's)
8. Provide good post-resuscitation care after ROSC (Return of spontaneous circulation = pulsatile rhythm)
9. Continue AHLR
- as long as possible. has shocking rhythm
- for passport. shows signs of life (moves, coughs, starts breathing normally or has a palpable pulse)
- until you are convinced for medical reasons that the resuscitation attempt will not be successful
- until you are convinced that it is ethically wrong to continue
The AHLR algorithm as a poster; see chapter 8, appendix 2.
7. After resuscitation
Post resuscitation care. Studies have shown that survival after successful resuscitation depends on optimal treatment after the heart has restarted (Return Of Spontaneous Circulation = ROSC).
Maintain high alertness for another cardiac arrest or other complications. Heart rhythm disturbances can often occur when the heart starts working again and the tissue gets good circulation again, especially if you have given medicine that thins the blood (reperfusion arrhythmias). Leave the defibrillation pads on the patient and keep the defibrillator connected at all times. Monitor the patient closely all the way to hospital.
Do the diagnostics you have available. Take a 12-lead EKG when you can. This can, among other things, provide information on whether a heart attack is the cause of the cardiac arrest. A possible heart attack is treated in consultation with the doctor on duty. Measure blood sugar and temperature. Look for correctable causes (the four H's and the four T's).
Provide treatment:
- Ventilate the patient until he/she starts breathing on his/her own. You must ventilate 10-12 times per minute. Be careful, it is harmful both to ventilate too much and too little. It is best to monitor this with a capnograph. EtCO2 must lie between 4.5kPa and 5.5kPa.
- If the patient is still unconscious 5 minutes after the cardiac arrest and he/she is between 18 and 80 years old, consider cooling! This is done by placing ice packs in the neck, armpits and groin. In hospital, this treatment continues, but the TTM study shows that it is not known what is best between 33 and 36 degrees. The most important thing is not to overheat. to normotemp/above 36 degrees. It has been documented in large studies that such hypothermia treatment both results in more survivors and better results in terms of brain function after a cardiac arrest.
- Consider the use of medication in collaboration with the doctor on duty. Acetylsalicylic acid, beta blockers, Plavix, Klexane, Atropine, Cordarone, thrombolysis and others are relevant.
8. Attachments and references
Attachments
- The Norwegian Resuscitation Council's summary of the AHLR guidelines from 2015.
- AHLR algorithm. This is copyright protected and you must download it yourself from www.nrr.org (Click on "Downloadable CPR posters for personal use").
References:
- ERC guidelines 2015 and associated articles. www.erc.edu
- 2. AHLR. Norwegian basic course in advanced cardiopulmonary resuscitation. Norwegian Resuscitation Council. www.nrr.org
- 3. AHLR – Norwegian guidelines 2015. Norwegian Resuscitation Council. www.nrr.org


All comments are moderated before being published. Your email will not be visible